Mild traumatic brain injury: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
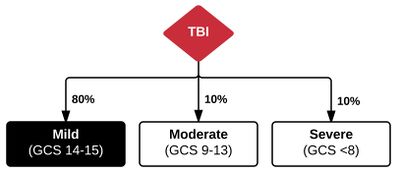
[[File:Mild TBI.JPG|400px]] | [[File:Mild TBI.JPG|400px]] | ||
*Concussion (mild TBI) | *Concussion (mild TBI) | ||
**GCS 14-15 | |||
**Neurologic dysfunction that varies without gross lesions (ie patients have trouble with memory, attention, and executive functioning | |||
**Occurs after a blunt force or acceleration-deceleration [[head injury]] | |||
**Likely secondary to metabolic insult ie low oxygen state, ion changes | |||
**Structural imaging on MRI or CT might not indicate any injury | |||
**Often evidence on microscopic level of injury with histology | |||
**Important to not expose the already injured brain to repeated insults which is why there are usually worsening symptoms after a repeat concussion | |||
*Types | *Types | ||
**Simple concussion | **Simple concussion | ||
| Line 9: | Line 17: | ||
***Symptoms with exertion | ***Symptoms with exertion | ||
== | ==Clinical Signs and Symptoms== | ||
*Most consistent abnormality is subtle impairments in cognitive function | *Most consistent abnormality is subtle impairments in cognitive function | ||
**Attention, concentration, memory, processing speed, reaction time | **Attention, concentration, amnesia, memory, processing speed, reaction time, calculation, executive function | ||
*Physical signs/symptoms | *Physical signs/symptoms | ||
**[[Headache]], dizziness, insomnia, fatigue, uneven gait, nausea/[[vomiting]], blurred vision, [[seizure]] | **[[Headache]], dizziness, insomnia, fatigue, uneven gait, nausea/[[vomiting]], blurred vision, [[seizure]] | ||
*Behavioral changes | *Behavioral changes | ||
**Irritability, depression, anxiety, sleep disturbances, problems related to school/work | **Irritability, depression, anxiety, sleep disturbances, problems related to school/work, emotional lability, loss of initiative, loneliness and helplessness | ||
==Evaluation== | |||
*No reliable test that can confirm diagnosis of concussion | |||
*Clinical Signs and Symptoms may occur immediately or be delayed by days-weeks | |||
*Important to document full examination and should do gait and congnition testing | |||
**Mini Mental State Exam | |||
**Standardized Assessment for Concussion | |||
***Takes 10-15 mins to administer often not performed in ED | |||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
{{Intracranial hemorrhage DDX}} | {{Intracranial hemorrhage DDX}} | ||
==Management== | ==Management== | ||
| Line 33: | Line 46: | ||
==Disposition== | ==Disposition== | ||
* | *Given good follow up instructions detailing a graded return-to-activity program and symptoms to anticipate during recovery <ref>Ronsford J, et al. Impact of early intervention on outcome after mild traumatic head in adults. 2002</ref> | ||
*Discharge patient to care of responsible individual | |||
*Patients might not understand discharge instructions so repeat them to the individual taking care of the patient | |||
*Recommend strict rest for 1-2 days with gradual introduction back to regular activity<ref>Thomas DG, Apps JN, Hoffmann RG, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015; 2(135):213-223.</ref> | *Recommend strict rest for 1-2 days with gradual introduction back to regular activity<ref>Thomas DG, Apps JN, Hoffmann RG, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015; 2(135):213-223.</ref> | ||
*Physical activity at any level (light aerobic, moderate, full) within first 7 days compared with no activity associated with lower rates of persistent symptoms at 28 days (29% vs. 40%)<ref>Grool AM et al. Association Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and Adolescents. JAMA. 2016;316(23):2504-2514.</ref> | *Physical activity at any level (light aerobic, moderate, full) within first 7 days compared with no activity associated with lower rates of persistent symptoms at 28 days (29% vs. 40%)<ref>Grool AM et al. Association Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and Adolescents. JAMA. 2016;316(23):2504-2514.</ref> | ||
| Line 40: | Line 55: | ||
==Prognosis== | ==Prognosis== | ||
*At 3 mo after injury | *At 3 mo after injury 20-40% are symptomatic | ||
**with treatment for the most common symptoms of headache, difficulty concentrating and short-term memory difficulties being rest and in some circumstances NSAIDS. | |||
*At 1 yr after injury 15% are symptomatic | *At 1 yr after injury 15% are symptomatic | ||
==Post Concussive Syndrome== | |||
*Most common symptoms | |||
**Headache | |||
**Dizziness | |||
**Decreased concentration | |||
**Memory problems | |||
**Sleep Disturbance | |||
**Irritability | |||
**Fatigue | |||
**Visual disturbances | |||
**Judgment problems | |||
**Depression | |||
**Anxiety | |||
*Cluster of symptoms becomes chronic ie for 6 weeks | |||
*Diagnosed w/ | |||
**Neuropsychological testing | |||
**Symptom checklist | |||
*Treated with symptom management | |||
**Appropriate referral to TBI clinic or Neuropsychologist | |||
==See Also== | ==See Also== | ||
Revision as of 21:03, 7 July 2017
Background
- Concussion (mild TBI)
- GCS 14-15
- Neurologic dysfunction that varies without gross lesions (ie patients have trouble with memory, attention, and executive functioning
- Occurs after a blunt force or acceleration-deceleration head injury
- Likely secondary to metabolic insult ie low oxygen state, ion changes
- Structural imaging on MRI or CT might not indicate any injury
- Often evidence on microscopic level of injury with histology
- Important to not expose the already injured brain to repeated insults which is why there are usually worsening symptoms after a repeat concussion
- Types
- Simple concussion
- Gradual resolution of symptoms within 7-10d
- Complex concussion
- Persisting symptoms or cognitive impairment
- Symptoms with exertion
- Simple concussion
Clinical Signs and Symptoms
- Most consistent abnormality is subtle impairments in cognitive function
- Attention, concentration, amnesia, memory, processing speed, reaction time, calculation, executive function
- Physical signs/symptoms
- Behavioral changes
- Irritability, depression, anxiety, sleep disturbances, problems related to school/work, emotional lability, loss of initiative, loneliness and helplessness
Evaluation
- No reliable test that can confirm diagnosis of concussion
- Clinical Signs and Symptoms may occur immediately or be delayed by days-weeks
- Important to document full examination and should do gait and congnition testing
- Mini Mental State Exam
- Standardized Assessment for Concussion
- Takes 10-15 mins to administer often not performed in ED
Differential Diagnosis
Intracranial Hemorrhage Types
- Intra-axial
- Hemorrhagic stroke (Spontaneous intracerebral hemorrhage)
- Traumatic intracerebral hemorrhage
- Extra-axial
- Epidural hemorrhage
- Subdural hemorrhage
- Subarachnoid hemorrhage (aneurysmal intracranial hemorrhage)
Management
- Simple
- Limitations on playing and training while symptomatic
- Follow up with primary care provider
- Complex
- Refer to sports medicine or concussion specialist
Disposition
- Given good follow up instructions detailing a graded return-to-activity program and symptoms to anticipate during recovery [1]
- Discharge patient to care of responsible individual
- Patients might not understand discharge instructions so repeat them to the individual taking care of the patient
- Recommend strict rest for 1-2 days with gradual introduction back to regular activity[2]
- Physical activity at any level (light aerobic, moderate, full) within first 7 days compared with no activity associated with lower rates of persistent symptoms at 28 days (29% vs. 40%)[3]
- Multicohort study - 2400 children, aged 5-18, in the emergency department
- Still recommend strict rest for first 24-48 hours
Prognosis
- At 3 mo after injury 20-40% are symptomatic
- with treatment for the most common symptoms of headache, difficulty concentrating and short-term memory difficulties being rest and in some circumstances NSAIDS.
- At 1 yr after injury 15% are symptomatic
Post Concussive Syndrome
- Most common symptoms
- Headache
- Dizziness
- Decreased concentration
- Memory problems
- Sleep Disturbance
- Irritability
- Fatigue
- Visual disturbances
- Judgment problems
- Depression
- Anxiety
- Cluster of symptoms becomes chronic ie for 6 weeks
- Diagnosed w/
- Neuropsychological testing
- Symptom checklist
- Treated with symptom management
- Appropriate referral to TBI clinic or Neuropsychologist
See Also
References
- ↑ Ronsford J, et al. Impact of early intervention on outcome after mild traumatic head in adults. 2002
- ↑ Thomas DG, Apps JN, Hoffmann RG, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015; 2(135):213-223.
- ↑ Grool AM et al. Association Between Early Participation in Physical Activity Following Acute Concussion and Persistent Postconcussive Symptoms in Children and Adolescents. JAMA. 2016;316(23):2504-2514.