Marfan syndrome: Difference between revisions
| Line 65: | Line 65: | ||
[[Category:Misc/General]] | [[Category:Misc/General]] | ||
===Differential Diagnosis=== | |||
* Classic vs. Kyphoscoliotic vs. [https://marfan.org/conditions/veds/ Vascular Ehlers-Danlos Syndrome (vEDS)] | |||
* [https://marfan.org/conditions/loeys-dietz/ Loeys-Dietz Syndrome (LDS)] | |||
* Familial Thoracic Aortic Aneurysm and Dissection (FTAAD) | |||
* Familial Ectopia Lentis Syndrome | |||
* MASS Phenotype (Myopia, Mitral Valve Prolapse, Aortic Root Dilatation, Aortic Aneurysm Syndrome, Striae, Skeletal Findings) | |||
* Shprintzen-Goldberg Syndrome | |||
* Beals Syndrome | |||
* Stickler Syndrome | |||
* Non-Specific Connective Tissue Disorder | |||
===Evaluation=== | |||
'''Initial evaluation often occurs in the outpatient setting and involves:''' | |||
** Thorough physical exam for identification of classically associated features | |||
** Review of family medical history | |||
** Slit lamp dilated pupil eye exam (to evaluate for ectopia lentis) | |||
** Echocardiogram | |||
** Advancement to specialist involvement, review of transthoracic echocardiography for aortic root dilation / aneurysm / heart valve involvement, potential genetic testing and/or medical genetics consultation per current guidelines<ref>Reference 5 details here.</ref> | |||
'''Acute Aortic Syndrome (AAS)''' | |||
* A high index of suspicion for AAS in the ED setting is critical in MFS when symptoms or signs of this life-threatening complication occur. | |||
* '''Key Elements:''' | |||
** Sudden onset of severe, “thunderclap” quality, potentially “tearing” and/or migratory chest, neck, abdominal, and/or back pain | |||
** Young patients with few traditional cardiovascular risk factors | |||
** Current or recent pregnancy | |||
** Family history of aortic aneurysm/dissection or unexplained sudden death | |||
** Typical “Marfanoid” features may not always be present, especially in non-white patients | |||
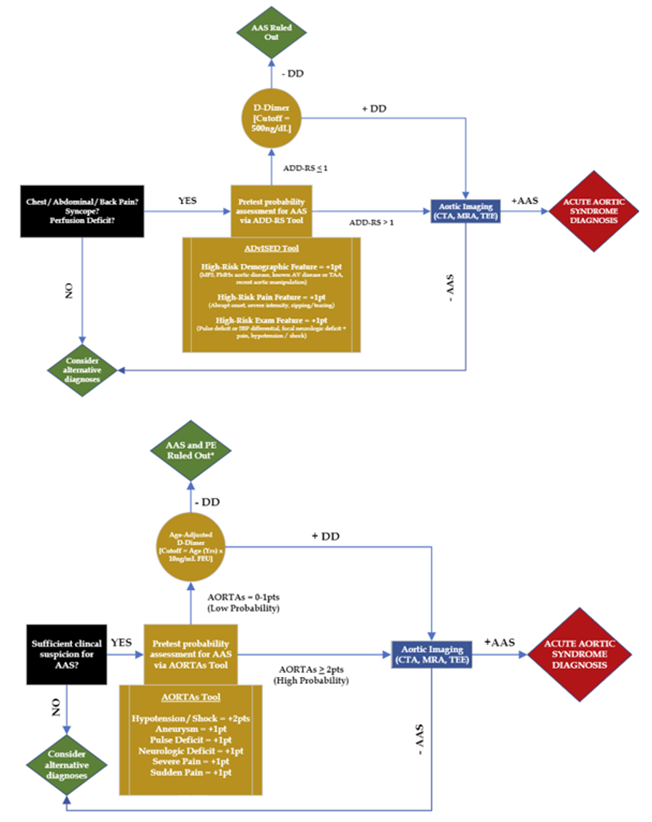
* Clinical decision-making tools and algorithms are available (e.g., ADvISED Trial ADD-RS + D-dimer, AORTAs Algorithms), but are not yet externally validated (see Figure 3, Table 1)<ref>Reference 6 details here.</ref> | |||
* Basic labs, troponin, D-dimer | |||
** '''Important Note:''' D-dimer is not 100% sensitive and cannot exclude all acute aortic syndromes | |||
* EKG, CXR | |||
* CTA / MRA aortic protocol (with IV contrast) | |||
* Bedside POCUS | |||
** Left ventricular outflow tract, aortic root, aortic valve, pericardium, abdominal aorta survey | |||
* Formal TTE / TEE | |||
'''Other Emergencies''' | |||
* Standard workup as with non-MFS patients | |||
[[File:ASvISED_Trial_Algorithm_and_AORTAs_Algorithm.png|thumb|center|800px|'''Figure 3.''' TOP: (Figure 1 from Peña et al. (2022) – flowchart of ADvISED Trial Algorithm). | |||
BOTTOM: (Figure 2 from Peña et al. (2022) – flowchart of AORTAs Algorithm).]] | |||
[[File:Pena Summary.png|thumb|center|800px|'''Table 1.''' Summary from Peña et al. (2022) of currently published clinical tools for acute aortic syndrome in the ED, with respective components and scoring systems.]] | |||
Revision as of 16:20, 25 August 2025
Background
- Marfan syndrome (MFS) is a heritable connective tissue disorder with multi-system involvement
- First characterized as a syndrome by French pediatrician Antoine Marfan in 1896
- Clinical features vary along a spectrum typical of autosomal-dominant disorders
- Autosomal-dominant mutation in FBN1 gene (encodes collagen matrix protein fibrillin-1) on chromosome 15
- This results in cystic medial degeneration of the aortic tunica media (leading to increased risk of aortic aneurysm / dissection)
- This also interferes with elastin deposition during extracellular matrix formation implicates in the elasticity of multiple tissue types
- Majority of cases (75%) are familial / inherited vs. minority (25%) are de novo mutations
- Estimated prevalence of 1/5000 individuals worldwide (equal between men and women)
- Life expectancy for those diagnosed and treated is now close to that of non-MFS population (previously expected increase in patient mortality by third and fourth decades of life)
Clinical Features & Diagnostic Criteria
Revised Ghent Nosology (2010)[2]
In the absence of family history:
- Aortic Root Dilatation Z Score > 2 and Ectopia Lentis
- Aortic Root Dilatation Z Score > 2 and FBN1 Mutation
- Aortic Root Dilatation Z Score > 2 and Systemic Score > 7 points
- Ectopia Lentis and FBN1 Mutation (associated with aortic root dilatation)
In the presence of family history:
- Ectopia Lentis and Family History of Marfan Syndrome (MFS)
- Systemic Score > 7 points and Family History of MFS
- Aortic Root Dilatation:
* Z Score > 2 (if age > 20 years) * Z Score > 3 (if age < 20 years) and Family History of MFS
Clinical Features (not all may be present)
- Tall stature, long extremities
- Reduce upper-to-lower segment ratio, increased arm span-to-height ratio
- Arachnodactyly (“wrist sign, thumb sign), reduced elbow extension
- Scoliosis or thoracolumbar kyphosis
- Pectus excavatum or carinatum
- Ligamentous laxity, hyperextensibility
- Protrusio acetabuli
- Hindfoot deformity, plain flat foot
- Ectopia lentis
- Myopia (often severe); retinal detachment
- Lumbrosacral dural ectasia
- Dolichocephaly, downward slanting palpebral fissures, enophthalmos, retrognathia, malar hypoplasia, high arched palate
- Skin striae
Increased risk of:
- Acute Aortic Syndrome (AAS)
- Thoracic aortic aneurysm
- Stanford Types A and B Aortic Dissection
- Intramural Hemotoma (IMH)
- Mitral valve prolapse (present in up to 60%) and mitral regurgitation
- Spontaneous pneumothorax (associated with bullae, 4-11%)
- Subarachnoid hemorrhage (SAH)
- Controversial link between Marfan Syndrome and intracranial aneurysms (more clearly associated with vEDS and LDS)
- Ocular Lens dislocation, retinal detachment
- Spinal conditions (scoliosis; lumbosacral disease; dural ectasia)
- Musculoskeletal injuries due to joint laxity (laxity in 85% of children, 56% of adults)
- Complications during pregnancy (risk of aortic dissection)
- Type A dissection risk increases with aortic dilation; Type B risk poorly understood. (aortic dissection in up to 4.5%, primarily peripartum)
Differential Diagnosis
- Classic vs. Kyphoscoliotic vs. Vascular Ehlers-Danlos Syndrome (vEDS)
- Loeys-Dietz Syndrome (LDS)
- Familial Thoracic Aortic Aneurysm and Dissection (FTAAD)
- Familial Ectopia Lentis Syndrome
- MASS Phenotype (Myopia, Mitral Valve Prolapse, Aortic Root Dilatation, Aortic Aneurysm Syndrome, Striae, Skeletal Findings)
- Shprintzen-Goldberg Syndrome
- Beals Syndrome
- Stickler Syndrome
- Non-Specific Connective Tissue Disorder
Evaluation
Initial evaluation often occurs in the outpatient setting and involves:
- Thorough physical exam for identification of classically associated features
- Review of family medical history
- Slit lamp dilated pupil eye exam (to evaluate for ectopia lentis)
- Echocardiogram
- Advancement to specialist involvement, review of transthoracic echocardiography for aortic root dilation / aneurysm / heart valve involvement, potential genetic testing and/or medical genetics consultation per current guidelines[1]
Acute Aortic Syndrome (AAS)
- A high index of suspicion for AAS in the ED setting is critical in MFS when symptoms or signs of this life-threatening complication occur.
- Key Elements:
- Sudden onset of severe, “thunderclap” quality, potentially “tearing” and/or migratory chest, neck, abdominal, and/or back pain
- Young patients with few traditional cardiovascular risk factors
- Current or recent pregnancy
- Family history of aortic aneurysm/dissection or unexplained sudden death
- Typical “Marfanoid” features may not always be present, especially in non-white patients
- Clinical decision-making tools and algorithms are available (e.g., ADvISED Trial ADD-RS + D-dimer, AORTAs Algorithms), but are not yet externally validated (see Figure 3, Table 1)[2]
- Basic labs, troponin, D-dimer
- Important Note: D-dimer is not 100% sensitive and cannot exclude all acute aortic syndromes
- EKG, CXR
- CTA / MRA aortic protocol (with IV contrast)
- Bedside POCUS
- Left ventricular outflow tract, aortic root, aortic valve, pericardium, abdominal aorta survey
- Formal TTE / TEE
Other Emergencies
- Standard workup as with non-MFS patients