WLA VA:COVID19: Difference between revisions
Mceledon83 (talk | contribs) |
Mceledon83 (talk | contribs) |
||
| Line 36: | Line 36: | ||
[[File:Ro example.png|center|Ro Example]] | [[File:Ro example.png|center|Ro Example]] | ||
=== Clinical Findings === | |||
* At onset: fever, dry cough, myalgias, fatigue, shortness of breath | |||
** Fever and cough start early, SOB noted about 9 days into illness | |||
** Fever not present in all adults (less common in vulnerable populations) | |||
** Less common: cough with sputum, sore throat, headache, congestion, GI symptoms | |||
* Most common complications: pneumonia, ARDS (avg 8 days from onset, 20% of patients in China) | |||
** Decompensation risk occurs during 2nd week of illness | |||
* Risk factors: older adults, underlying conditions (lung disease, heart disease, diabetes) | |||
** Children: milder disease (see Children) | |||
** Pregnant patients: don’t appear to be at increased risk of infection or adverse outcomes (limited data - see Pregnant Women) | |||
==== Laboratory Findings ==== | |||
* Lymphopenia most common in critically ill; mildly elevated ALT, AST; normal pro-calcitonin on admission | |||
** Elevated d-dimer and severe lymphopenia are associated with increased mortality | |||
** RT-PCR is currently test of choice for confirming cases | |||
*** Test kit availability is currently limited as of mid March | |||
*** Consider influenza/viral respiratory panel to identify alternative diagnoses | |||
**** Although co-infection is possible | |||
==== Imaging ==== | |||
* XRay: | |||
** Portable CXR preferred in PUI to prevent spread of infection | |||
** May be normal in early disease | |||
** Typical pattern is peripheral patchy ground glass opacities (GGO) | |||
** More opacities correlates with worse disease | |||
** GGOs may coalesce and appear as infiltrates | |||
* CT: | |||
* Many have normal imaging early on (so CDC DOES not recommend CT for diagnostic purposes at this time) | |||
** CT (86%) more sensitive than CXR (59%) for detecting GGOs | |||
** Radiopaedia COVID-19 Resources (https://radiopaedia.org/articles/covid-19) | |||
** From the American College of Radiology (3/11/20): “Generally, the findings on chest imaging in COVID-19 are not specific, and overlap with other infections, including influenza, H1N1, SARS and MERS. Being in the midst of the current flu season with a much higher prevalence of influenza in the U.S. than COVID-19, further limits the specificity of CT.” | |||
* Reinfection (after recovery from COVID19): unclear if possible | |||
** Limited data. Unlikely to be reinfected shortly after but unknown about later on | |||
==General Prevention Recommendations== | ==General Prevention Recommendations== | ||
Revision as of 02:22, 18 March 2020
Introduction
- Disease name = COVID-19
- Virus = SARS-CoV-2 (previously 2019-nCoV
Virology
- Coronaviruses are a common human pathogens (discovered in the1960s to cause the common cold).
- During epidemics, they are the cause of up to one-third of community-acquired upper respiratory tract infections in adults; may cause diarrhea in infants and children as well)
- SARS-CoV-2 is a novel coronavirus (a new strain not previously identified in humans)
- Likely primary source = bats
- A betacoronavirus in the same subgenus as the severe acute respiratory syndrome (SARS) virus
- Receptor-binding gene region is very similar to that of the SARS coronavirus (uses angiotensin-converting enzyme 2 [ACE2] for cell entry)
- Middle East respiratory syndrome (MERS) virus, another betacoronavirus, appears more distantly related
- Viral survival time of SARS-CoV-2:
- Stainless steel: persists for 3 hours (or longer)
- Underscores the importance of environmental cleaning / disinfection
- Cleaning gets rid of the proteins that would interfere with a disinfectants effectiveness
- Note: studied in a simulated lab environment. Lab virions not covered in protein and mucus and other things that would mimic real life and that could prolong survival
Basic Epidemiology/Infectivity Data
- Expected patient outcomes (from data so far):
- 80% have mild symptoms
- 15% have severe disease requiring hospitalisation
- 5% require mechanical ventilation
- Case fatality rate (CFR) = 2-4% (from Hubei data)
- SARS ~ 10%
- MERS ~ 35%
- Seasonal flu ~ 0.1-0.2%
- 1918 Pandemic Influenza ~ 2-3%
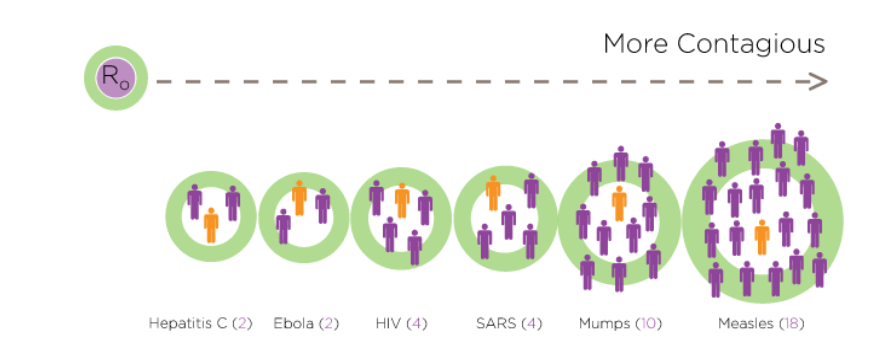
- R0 = 2.2 - 4.2
- Where R0 = expected number of secondary cases produced by a single typical infection in a susceptible population (basic reproductive rate)
- R0 for seasonal flu ~ 1.3
- R0 for pandemic flu ~ 1.5-1.8
- Incubation: 5 days (median); range of 2-14 days
- Serial interval duration = 7.5 days
- Serial interval refers to the time from illness onset in successive cases in a transmission chain
Clinical Findings
- At onset: fever, dry cough, myalgias, fatigue, shortness of breath
- Fever and cough start early, SOB noted about 9 days into illness
- Fever not present in all adults (less common in vulnerable populations)
- Less common: cough with sputum, sore throat, headache, congestion, GI symptoms
- Most common complications: pneumonia, ARDS (avg 8 days from onset, 20% of patients in China)
- Decompensation risk occurs during 2nd week of illness
- Risk factors: older adults, underlying conditions (lung disease, heart disease, diabetes)
- Children: milder disease (see Children)
- Pregnant patients: don’t appear to be at increased risk of infection or adverse outcomes (limited data - see Pregnant Women)
Laboratory Findings
- Lymphopenia most common in critically ill; mildly elevated ALT, AST; normal pro-calcitonin on admission
- Elevated d-dimer and severe lymphopenia are associated with increased mortality
- RT-PCR is currently test of choice for confirming cases
- Test kit availability is currently limited as of mid March
- Consider influenza/viral respiratory panel to identify alternative diagnoses
- Although co-infection is possible
Imaging
- XRay:
- Portable CXR preferred in PUI to prevent spread of infection
- May be normal in early disease
- Typical pattern is peripheral patchy ground glass opacities (GGO)
- More opacities correlates with worse disease
- GGOs may coalesce and appear as infiltrates
- CT:
- Many have normal imaging early on (so CDC DOES not recommend CT for diagnostic purposes at this time)
- CT (86%) more sensitive than CXR (59%) for detecting GGOs
- Radiopaedia COVID-19 Resources (https://radiopaedia.org/articles/covid-19)
- From the American College of Radiology (3/11/20): “Generally, the findings on chest imaging in COVID-19 are not specific, and overlap with other infections, including influenza, H1N1, SARS and MERS. Being in the midst of the current flu season with a much higher prevalence of influenza in the U.S. than COVID-19, further limits the specificity of CT.”
- Reinfection (after recovery from COVID19): unclear if possible
- Limited data. Unlikely to be reinfected shortly after but unknown about later on
General Prevention Recommendations
- Exercise general infection precautions
- Person-to-person transmission occurs with close contact (6 feet)
- Direct contact with mucous membranes or respiratory droplets
- Indirect: cough —> secretions left on surface —> 2nd person touches surface secretions and touches face & mucous membranes
- Avoid touching your face (try it, it’s not easy)
- Frequent Handwashing
- Alcohol based hand sanitizer
- Diligent hand wasing
- 20 seconds minimum
- Image shows commonly forgotten areas: thumb (ulnar aspect), fingertips, WRIST (Borrowed from WHO Hand Hygiene for Healthcare)
- Wear a mask if you develop respiratory symptoms (fever, cough, rhinorrhea, congestion) to prevent spread
- Person-to-person transmission occurs with close contact (6 feet)
- Avoid unnecessary travel
- Stay home if symptomatic
- Home care does not mean being out in the parks with other groups of people
- Contact your supervisor: due to expected HCW shortages, minor symptoms may be allowed to continue working with adequate PPE to prevent infection spread
Precautions For Healthcare Workers
PPE Bottom Line: Per CDC and LADPH (3.12.20)
- “Can collect specimens (e.g., nasopharyngeal swabs) for COVID-19 observing standard, contact, and droplet precautions including eye protection in a normal examination room with the door closed”
- No airborne isolation required (unless aerosol-generating procedure)
Transmission
- Simply walking into a room is NOT a recognized risk of transmission. Must make contact with respiratory droplet (directly or indirectly)
- Masks: MOST IMPORTANT utility is to put on the coughing individual
- Research clearly demonstrates it decreases shedding of infectious material in the environment
- This is more effective than HCWs wearing masks prophylactically to prevent catching the infection when not actually performing close contact patient care
- How long to shut a patient room down after a COVID patient is in there?
- It’s not about the risk of contracting the infection but about the ability to clean room safely without respiratory protection precautions by the cleaner
- 30-40 minutes usually sufficient (for most modern facilities) as long as no aerosol-generating procedure performed (longer, time not clearly stated at this time)
- Most modern rooms designed to have 12 air exchanges per hour
- Ventilation symptoms vary. So, older / fewer exchanges per hour => more time.
PPE Guidelines
- EVERY PATIENT CONTACT: Respiratory droplet precautions. Contact precautions also recommended but if gowns in short supply consider reserving for aerosol-generating procedures
- Droplet = surgical mask, eye protection
- Contact = gown and gloves
- Technique:
- Mask donning (often incorrectly done):
- Wash hands BEFORE touching mask
- Grip mask by loops/bands/ties only
- Coloured portion typically faces outward
- Mold / pinch the stiff edge to the shape of your nose
- Pull the bottom of the mask over your mouth AND chin
- Make sure you are up to date with fit testing
- Mask removal:
- Wash hands BEFORE touching mask
- Only make contact with the loops/bands/ties. DON’T TOUCH THE MASK ITSELF!
- Mask donning (often incorrectly done):
- For AEROSOL GENERATING procedures: airborne precautions (N95/PAPR)
- Due to higher risk of aerosolizing droplets-- infection itself doesn’t seem to be spread via airborne route)
- Aerosol generating procedures (avoid when possible)
- Bag-valve mask (BMV)
- CPAP/BiPAP
- Intubation
- Nebulizer administration (COMMONLY FORGOTTEN) - use MDI instead. E.g. 8-12 MDI puffs instead of albuterol 2.5-5mg INH.
- Bronchoscopy
- Chest PT
PPE Shortage/Limiting Usage Guidelines
In case of PPE shortage or in an attempt to save on PPE supplies, the following guidelines were approved by CDC 3/13/20
- Same respirator can be worn for multiple serial patient contacts (e.g. in between successive COVID/PUI (patients under investigation) without exchanging respirator. Therefore, in between each patient:
- No need to change mask or eye protection
- BUT need to change gown and gloves
- Respirator reuse possible? Higher risk because of having to touch the mask and either self-inoculate or transmit to another patient (e.g. wear it for a patient, then you remove, and then you put it back on)
- If you must do this because of limited supplies, don and doff properly and perform proper hand hygiene in between
- CDC / NIOSH will allow certain N95s to be used beyond manufacture-designated shelf life
- See list of appropriate models here (manufactured between 2003-2013)
- N95 Reuse? Probably okay to re-use same N95 during an 8 hour shift as long as no tears or visible contamination. Store facedown in labeled re-sealable bag/container.
- Based on non peer reviewed reports from Washington State
Healthcare Worker Monitoring
- Every HCW should be keeping a thermometer at home
- Self-monitor BID (and especially before work). Facilities should screen their HCW prior to shifts.
- If symptomatic, notify supervisor.
- If febrile, STAY HOME.
- If other symptoms, discuss with supervisor / clinical experts. Due to expected HCW shortages, minor symptoms may be allowed to continue working with adequate PPE to prevent infection spread