The difficult airway
Revision as of 00:46, 25 December 2014 by Chrismathew92 (talk | contribs)
LEMON Mnemonic
LOOK
- Look at the patient externally for characteristics that are known to cause difficult laryngoscopy,
intubation or ventilation[1]
- Trauma
- Short neck
- Micrognathia
- Prior surgery
- May also be difficult to bag
- Body mass index
- Advanced age
- Beard
- No teeth
- Snoring
Evaluate 3-3-2-1
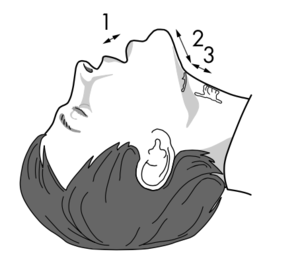
- Ideally the distance between the patient's incisor teeth should be at least 3 finger breadths (3), distance between the hyoid bone and the chin should be at least 3 finger breadths (3), distance between the thyroid notch and the floor of the mouth should be at least 2 finger breadths (2). Lower jaw should not sublux more than 1cm (1).
Mallampati
- The patient sits upright, opens mouth and protrudes tongue
- Grades are based on visibility of the uvula, posterior pharynx, hard, and soft palate
Obstruction
- Assess for conditions leading to airway obstruction such as peritonsillar abscesses, trauma, or epiglottitis.
Neck Mobility
- Patient places chin down onto their chest and extend their neck. Remove the hard collar and provide manual stabilization in trauma patients. Poor neck mobility impacts ability to have airway access alignment.
ASA DIFF AIRWAY ALGORITHM
- Does not necessary apply to the Emergency Department since the patient can always be awakened and case cancelled
- Cricothyrotomy should always be the last step in patients with failure to oxygen and ventilate with BVM and inability to intubate
- Straight blade- Miller- may offer better manipulation of a large epiglottis in children or for micrognathia or "buck teeth"
Airway Adjuncts
Gum Bougie
Blind orotracheal intubation
Blind Naso Trach Intubation
- Not as successful but still an option
- Higher complication rate- bleeding, emesis, and airway trauma
Do not attempt in patients with posterior pharyngeal swelling such as in angioedema
Lighted Optical Stylets
- High success rate- esp good for trauma, cspine
- Use for both reg and nasotrach
- Low complication rate
- Limited by fogging, secretion, recognition of anatomy, cost, and rare provider experience
LMA
- Can use without muscle relaxants
- Better than face mask
- Can be used as bridge to fiberoptic intubation
- Limited by unreliable seal at peak insp pressure
- Aspiration risk
- Mucosal trauma
- LMA better than endotracheal for paramedics, especially in pediatric patients[2][3]
- Itubating LMA (LMA-Fastrach) provides the opportunity to convert to a definitive airway after rescue with the supraglottic device
Combitube- esoph obturator
- Good for nurses and paramedics with limited intubation skill
- Indicated if diff airway predicted, can't see glottis with laryngoscope,
- Reduced risk for aspiration compared to face mask or LMA
- Can maintain spinal immobilization
- Large size predisposes to esoph dilatation and laceration as a complication
Trans Trach Jet Vent
- TTJV
- Needle through cric mem, connected to 50 psi 02- can ventilate and oxygenate ok
- Need adequate oxygen pressure
- 1 sec insp and 2- 3 sec exp to avoid breath stacking
- May get ptx or barotrauma
- Contraindications- distorted anatomy, bleeding diathesis, complete airway obstruction
Retrograde Intubation
- Perc guide wire through cric and retrograde intubation over wire
- Use guide catheter over wire and then ett
- Need time to set up
- Risk hematoma, ptx
- Contra- bleeding, distorted anatomy
Fiberoptic Bronchoscopic Intubation
- Takes time to set up
- Good for c-spine injury or awake pt with diff airway
- Go through nose
- Use for all ages, can give 02 during procedure thru fiberscope, immediate confirmation of position
- Limited by secretions, bleeding, poor suction,
Rigid Fiberoptic Laryngoscopes
- Use for diff airway or spinal immob
- Not as good and longer time to intubate than flex scope
Improving Passive Oxygenation
- Use in overweight, poor O2 reserve, hypoxia at baseline, concerns for rapid progression to hypoxia once apnea
- Pre oxygenate while sitting upright, only lay back once RSI drugs pushed.
- 30 degrees reverse trendelenburg position for intubation
- Nasal O2 while pre oxygenating and DURING intubation (after induction increase to 15L)
Surgical Airway
- can get subglottic stenosis
- rapid 4 step procedure faster but higher compl rate- cric cart fx
- can also do wire guided
- long term morbid, mortality similar to tracheostomy
See Also
Airway Pages
- Pre-intubation
- Induction
- Intubation
- Surgical airways
- Post-intubation
Source
- ↑ Rennie LM, Dunn MJG, et al. Is the ‘LEMON’ method an easily applied emergency airway assessment tool? European Journal of Emergency Medicine 2004;11:154–7
- ↑ Zhu X-Y, Lin B-C, Zhang Q-S, Ye H-M, Yu R-J. A prospective evaluation of the efficacy of the laryngeal mask airway during neonatal resuscitation. Resuscitation. 2011;82(11):1405–1409. doi:10.1016/j.resuscitation.2011.06.010
- ↑ Calkins MD, Robinson TD. Combat trauma airway management: endotracheal intubation versus laryngeal mask airway versus combitube use by Navy SEAL and Reconnaissance combat corpsmen. J Trauma. 1999;46(5):927–932