Deterioration after intubation: Difference between revisions
No edit summary |
|||
| Line 45: | Line 45: | ||
*Decrease TV | *Decrease TV | ||
*Increase sedation | *Increase sedation | ||
===Peak Vs Plateau Pressure=== | |||
*Super important to keep alveolar pressure low to prevent barotrauma | |||
*Peak Pressure is pressure of entire system (vent, ET tube, trachea, bronchus, bronchioles, alveoli). High peak pressure does not equal barotrauma | |||
*Plateau pressure - check with button on vent (may say plateau pressure or end-inspiratory hold) | |||
*High Peak and Normal Plateau - problem with vent, ET tube, bronchoconstriction (reactive airway disease/asthma/COPD). | |||
*High Peak and High Plateau - Compliance issue (pneumothorax, problem with alveoli like ARDS, fluid overload). Need to decrease pressure to prevent barotrauma. | |||
*Plateau pressures should be kept < 30mmHg if possible. | |||
[[File:ardsnet.jpg|thumb]] | |||
http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf | |||
[[File:ardsnet2.png|thumb]] | |||
Vent basics resource: https://emcrit.org/wp-content/uploads/2010/05/Managing-Initial-Vent-ED.pdf | |||
==See Also== | ==See Also== | ||
Revision as of 21:51, 21 March 2020
Background
- There are multiple reasons for a patient to deteriorate while on mechanical ventilation
- A systematic method of evaluating this deterioration is the best way to identify/fix the causative problem
Clinical Features
- Desaturation, other vital sign abnormalities, or cardiac arrest while on mechanical ventilation
Differential Diagnosis
DOPE[1][2]
- Displaced ETT
- Obstruction (anywhere along circuit)
- Pneumothorax
- Equipment failure (ventilator malfunction or disconnect)
Evaluation
- Clinical
Management
Troubleshoot
Immediately disconnect from ventilator (allows for expiration of stacked breaths)
- D - Displacement of tube or cuff
- Attach end-tidal CO2 to verify and check depth (cm at lip)
- O - Obstruction of tube/circuit
- Use suction catheter to remove mucus plug, or make sure patient not biting down, look for kink in tube
- P - Pneumothorax
- Verify via ultrasound, CXR, or needle thoracostomy (high suspicion)
- E - Equipment failure
- Connect to BVM
- S - Stacked breaths - Auto-PEEP especially in COPD/Asthma
- Disconnect from ventilator
Fix
- "DOTTS" Mnemonic
- D - Disconnect ventilator and put light pressure on patient chest
- O - Oxygen 100% BVM. Look for chest rise, listen and feel for cuff leak
- T - Tube position and patency. Pass bougie or suction all the way through tube to remove obstruction
- T - Tweak the vent. Usually need to decrease respiratory rate, decreased inspiratory time with changing E:I ratio (see below on breath-staking)
- S - Sonography and CXR
Auto-PEEP (Breath stacking) troubleshooting options
- Bronchodilators if COPD/asthma
- Decrease RR
- Decrease I:E ratio (increase expiratory time)
- Quicker inspiratory flow rate
- Decrease TV
- Increase sedation
Peak Vs Plateau Pressure
- Super important to keep alveolar pressure low to prevent barotrauma
- Peak Pressure is pressure of entire system (vent, ET tube, trachea, bronchus, bronchioles, alveoli). High peak pressure does not equal barotrauma
- Plateau pressure - check with button on vent (may say plateau pressure or end-inspiratory hold)
- High Peak and Normal Plateau - problem with vent, ET tube, bronchoconstriction (reactive airway disease/asthma/COPD).
- High Peak and High Plateau - Compliance issue (pneumothorax, problem with alveoli like ARDS, fluid overload). Need to decrease pressure to prevent barotrauma.
- Plateau pressures should be kept < 30mmHg if possible.
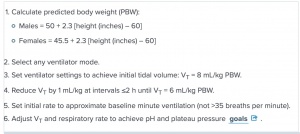
http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf
Vent basics resource: https://emcrit.org/wp-content/uploads/2010/05/Managing-Initial-Vent-ED.pdf
See Also
Mechanical Ventilation Pages
- Noninvasive ventilation
- Intubation
- Mechanical ventilation (main)
- Miscellaneous
External Links
References
- ↑ EMRA Critical Care Handbook
- ↑ Monica E. Kleinman et al. Pediatric Advanced Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. AAP. 2010. http://pediatrics.aappublications.org/content/126/5/e1361.full