Breast feeding jaundice
Background
- Breast feeding jaundice occurs within the first first week of life and overlaps with breast milk jaundice and physiologic jaundice.
- Is the result of inadequate breast milk volume and neonatal volume contraction relative to the amount of bilirubin.
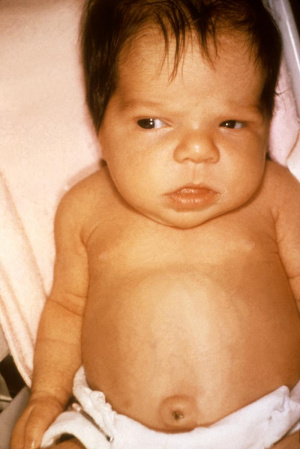
General neonatal jaundice features
- Jaundice within the first 4-7 days of life
- Scleral icterus
- Lethargy, if progression to severe elevation
- Unlikely when caused by a benign process (e.g. breast milk jaundice, breast feeding jaundice)
Differential Diagnosis
Indirect (Unconjugated) Hyperbilirubinemia
More common causes are listed first, followed by less common causes
- Breast milk jaundice
- Due to substances in milk that inhibits glucuronyl transferase. It may start as early as 3rd day and reaches peak by 3rd week of life. It is unlikely to cause kernicterus
- Breast feeding jaundice
- Patient does not receive adequate oral intake which then causes reduced bowel movement/bilirubin excretion. Best diagnosed by looking for signs of dehydration and comparing weight to birth weight.
- Blood group incompatibility: ABO, Rh factor, minor antigens
- Diabetic mother/gestational diabetes
- Internal hemorrhage
- Physiologic jaundice
- Polycythemia
- Sepsis
- Hemoglobinopathies: thalassemia
- Red blood cell enzyme defects: G6PD Deficiency, pyruvate kinase
- Red blood cell membrane disorders: spherocytosis, ovalocytosis
- Hypothyroidism
- Immune thrombocytopenic purpura
- Mutations of glucuronyl transferase (i.e., Crigler-Najjar syndrome, Gilbert syndrome)
Direct (Conjugated) Hyperbilirubinemia
Conjugated bilirubinemia implies a hepatic or post hepatic cause. More common causes are listed first.
- Hyperalimentation cholestasis
- Neonatal hepatitis
- Cytomegalovirus infection
- Sepsis
- TORCH infection (toxoplasma, other/syphilis, rubella, CMV, HSV)
- Biliary atresia
- Cystic fibrosis
- Hepatic infarction
- Inborn errors of metabolism (e.g., galactosemia, tyrosinosis)
Evaluation
Neonatal jaundice workup
The most important component of the workup is differention of direct vs indirect bilirubinemia
- Total and direct bilirubin levels ("neonatal bilirubin")
- CBC (for evaluation of hemolytic anemia or polycythemia vera)
- Consider coombs or T&S (mom & baby)
Neonatal jaundice diagnosis
- Determine if there are red flags or obvious diagnosis based on history and exam
- Mother's blood type (important if mother is RH negative or O blood type)
- Assess for any signs of decreasing oral intake or signs of dehydration?
- Baby's general appearance (well appearing? evidence of sepsis?)
- Determine bilirubinemia type: direct vs indirect
- Direct
- Admit
- Indirect
- Determine risk category
- See table below
- Determine if patient is above of below bilirubin cutoff by age and risk category
- See table below or use BiliTool or phototherapy guide
- Determine risk category
- Direct
Management
- The mother should supplement lack of breast milk with formula until quantity of milk increases
- Phototherapy may be necessary and the following chart and [BiliTool] can be used as a reference for treatment
Phototherapy guidelines for neonatal jaundice
| Age | Low Risk | Medium Risk | High Risk |
| Birth | 7.0 | 5.0 | 4.0 |
| 24h | 11.5 | 9.0 | 8.0 |
| 48h | 15 | 14 | 10 |
| 72h | 17.5 | 15 | 14 |
| 96h | 20 | 17.5 |
14.5 |
| 5+days | 21 | 17.5 | 15 |
- Low Risk: ≥38 weeks + no risk factors
- Medium Risk: (≥38 weeks + risk factors) or (35-37 weeks and no risk factors)
- High Risk: 35-37 weeks + risk factors
- Phototherapy is only used for an indirect hyperbilirubinemia
Disposition
- Bilirubin levels of 12 mg/dL (170 µmol/L) to 17 mg/dL can generally be rechecked within 24hrs and supplementation with formula
- Bilirubin levels of >17 mg/dL (294-430 µmol/L) should have phototherapy as well as formula supplementation while continuing breast feeding