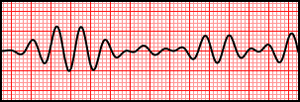
Polymorphic ventricular tachycardia
Background
- Form of ventricular tachycardia
- Multiple ventricular foci
- QRS complexes with varying morphology
- Subtypes include:
- Torsades de pointes
- bidirectional polymorphic VTach (as seen in digoxin toxicity)
Etiologies
- Myocardial ischemia (most common)
- Acquired or congenital prolonged QT
- TCAs, phenothiazines, Type I antiarrhythmics (quinidine, procainamide)
- Hypokalemia
- Hypomagnesemia
- Elevated intracranial pressure
- Brugada syndrome, short QT syndrome, congenital catecholaminergic polymorphic ventricular tachycardia
Clinical Features
- Syncope
- Palpitations
- Altered level of consciousness
- May present with cardiac arrest
Differential Diagnosis
Wide-complex tachycardia
Assume any wide-complex tachycardia is ventricular tachycardia until proven otherwise (it is safer to incorrectly assume a ventricular dysrhythmia than supraventricular tachycardia with abberancy)
- Regular
- Monomorphic ventricular tachycardia
- PSVT with aberrant conduction:
- PSVT with bundle branch block^
- PSVT with accessory pathway
- Atrial flutter with bundle branch block^
- Sinus tachycardia with bundle branch block^
- Accelerated idioventricular rhythm (consider if less than or ~120 bpm)
- Metabolic
- Irregular
- Atrial fibrillation/atrial flutter with variable AV conduction AND bundle branch block^
- Atrial fibrillation/atrial flutter with variable AV conduction AND accessory pathway (e.g. WPW)
- Atrial fibrillation + hyperkalemia
- Polymorphic ventricular tachycardia
^Fixed or rate-related
Evaluation
- Evaluate for underlying causes (e.g. electrolyte imbalances, ACS)
ECG Findings
- Wide QRS (>100ms or 3 small boxes)
- QRS complexes of varied amplitude, axis and duration
- Torsades: QRS complexes appear to twist around isoelectric line
- Rapid rhythm (usually 140-160 bpm, but can be up to 300 bpm)
- Irregular
Management
Pulseless
See Adult pulseless arrest and Pediatric pulseless arrest
Unstable
- Unsynchronized cardioversion (defibrillation) 200J (or 2J/kg for pediatrics)
- Correct any electrolyte abnormalities
Stable
- Correct any electrolyte abnormalities
- Torsades:
- Magnesium sulfate (for Torsades):
- 1-2gm IV, repeat in 5-15min; then 1-2gm/hr (3-10mg/min) drip
- Peds: 25-50mg/kg (max 2g) IV
- Isoproterenol, 2-8 mcg/min (if available)
- Overdrive Pacing to goal HR 90-120
- Note that this is only effective for preventing recurrence of TdP - it will not convert TdP to sinus rhythm
- Consider Lidocaine
- Avoid procainamide, amiodarone (may further prolong QT)
- Magnesium sulfate (for Torsades):
- Non-Torsades (baseline QT interval not prolonged)
- Amiodarone, agent of choice in setting of AMI or LV dysfunction
- 150 mg over 10min (15 mg/min), followed by 1 mg/min drip over 6hrs (360 mg total), then 0.5 mg/min drip over next 18 hrs (540 mg total)
- Peds: 5mg/kg (max 300mg), may repeat twice
- Procainamide
- 100 mg q5min until termination of arrhythmia, then start 2-6 mg/min (or 1-2 mg/min for renal/cardiac failure)
- Max dose 17mg/kg OR widening of QRS >50%
- Lidocaine, 1-1.5mg/kg IV q5min, repeat PRN up to 300mg/hr
- Beta-blockers (e.g. metoprolol 5mg IV q5m x 3) if blood pressure tolerates
- Amiodarone, agent of choice in setting of AMI or LV dysfunction
Refractory
- ≥3 episodes within 24 hours considered electrical storm
- May require alternate treatment (i.e. β-blockers, sedation, ablation)
Disposition
- Admit with cardiology consult, even if back in normal sinus rhythm
- Stable patients may be admitted to ward
- Pads should remain on patient's chest anticipating need for repeat cardioversion
- All patients should remain on telemetry or full cardio-respiratory monitoring for recurrent events
- Patients with features of instability or refractory VT are best admitted to CCU or ICU and may require urgent or emergent pacemaker placement
- Stable patients may be admitted to ward
See Also
- Tachycardia (wide)
- Torsades de pointes
- ACLS (Main), PALS (Main)
- Adult Pulseless Arrest, Pediatric pulseless arrest
- Critical care quick reference
- Nonsustained ventricular tachycardia