Sinusitis
Background
- Viral source is by far most common. Bacterial infection accounts for only 0.5-2% of all cases[1]
- Other causes include allergies and fungal infection
- Timeframe
- Acute (<4 weeks)
- Subacute (4-12 weeks)
- Chronic (>12 weeks)
Clinical Features
- Defined as 2 or more of the following:
- Blockage or congestion of nose
- Facial pain or pressure
- Hyposmia (diminished ability to smell)
- Anterior or posterior nasal discharge lasting <12wk
- Additional symptoms:
- Tooth pain
- Fever
- Sinus pressure while bending forward to changing head position
Clinical Features of Bacterial Sinusitis
- Symptoms persist >10 days
- Daytime cough
- Worsening or bimodal course
- Fever >102.2F (39C)
- Purulent nasal discharge >3d
- Pain in maxillary teeth
- Hx of diabetes
Clinical Features of Fungal Sinusitis
- Seen most often in immunocompromised individuals and poorly controlled diabetics
- Presents similarly to viral and bacterial sinusitis but symptoms worsen over time and do not improve with antibiotics
- See Mucormycosis
Differential Diagnosis
Rhinorrhea
- Upper respiratory infection, influenza
- Sinusitis
- Juvenile nasopharyngeal angiofibroma
- Nasal polyp
- Nasal mass
- Nasal foreign body
- CSF leak (e.g. basilar skull fracture)
- Toxic inhalation (e.g. selenium toxicity, neurotoxic shellfish poisoning)
Headache
Common
Killers
- Meningitis/encephalitis
- Myocardial ischemia
- Retropharyngeal abscess
- Intracranial Hemorrhage (ICH)
- SAH / sentinel bleed
- Acute obstructive hydrocephalus
- Space occupying lesions
- CVA
- Carbon monoxide poisoning
- Basilar artery dissection
- Preeclampsia
- Cerebral venous thrombosis
- Hypertensive emergency
- Depression
Maimers
- Giant cell arteritis of temporal artery (temporal arteritis)
- Idiopathic intracranial hypertension (Pseudotumor Cerebri)
- Acute Glaucoma
- Acute sinusitis
- Cavernous sinus thrombosis or cerebral sinus thrombosis
- Carotid artery dissection
Others
- Mild traumatic brain injury
- Trigeminal neuralgia
- TMJ pain
- Post-lumbar puncture headache
- Dehydration
- Analgesia abuse
- Various ocular and dental problems
- Herpes zoster ophthalmicus
- Herpes zoster oticus
- Cryptococcosis
- Febrile headache (e.g. pyelonephritis, nonspecific viral infection)
- Ophthalmoplegic migraine
- Superior Vena Cava Syndrome
Aseptic Meningitis
- Viral
- Tuberculosis
- Lyme disease
- Syphilis
- Leptospirosis
- Fungal (AIDS, transplant, chemotherapy, chronic steroid use)
- Noninfectious
Evaluation
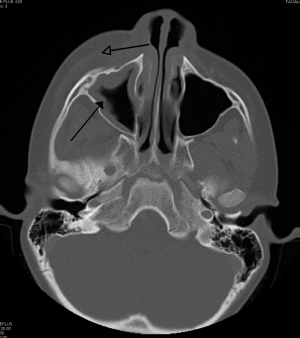
Maxillary sinusitis caused by a dental infection associated with periorbital cellulitis.
- Clinical diagnosis
- Consider CT only for toxic patients (to rule-out complication)
IDSA Guidelines 2012[2]
- Highlights identifying factors for acute bacterial vs. viral rhinosinusitis
- Concern for bacterial (treat with antibiotics) if any of these:
- Purulent discharge and pain on face or teeth > 10 days without improvement
- Severe symptoms or fever > 39 plus symptoms > 3 days
- "Double sickening" - sinusitis symptoms at end of initially improving URI that lasted > 5 days
Management
<10 days of symptoms
- Symptomatic treatment:
- Analgesia
- Mechanical irrigation with buffered, hypertonic saline
- OTC decongestants
- Intranasal decongestants (e.g. oxymetazoline for no more than 3 days)
- Intranasal corticosteroids (e.g. mometasone furoate monohydrate, Flonase)[3]
- Avoid antibiotics (Part of ACEP Choosing wisely)
>10 days of symptoms
- Possible bacterial source, especially if associated with:
- No clinical improvement after 10 days
- Severe symptoms or high fever and purulent nasal discharge or facial pain lasting for at least 3–4 consecutive days at the beginning of illness
- Onset with newly worsening that were initially improving (‘‘doublesickening’’)
- Acute bacterial sinusitis[4]
- Strep pneumo, non-typeable H. flu, Moraxella
- First line is amoxicillin-clavulanate for 7-10 days
- Amox 40-45mg/kg PO with clavulanate 3.2 mg/kg PO bid for 10d
- Second line is a respiratory fluoroquinolones (moxifloxacin, gemifloxacin, and levofloxacin) or doxycycline
- If allergic, can use cefdinir (7mg/kg PO bid) or cefuroxime (15 mg/kg PO bid)
Antibiotic Failure
- Obtain culture
- Consider nosocomial bacterial sinusitis (e.g. after prolonged nasotracheal intubation)
- Consider foreign body
- Consider antifungals
Disposition
- Discharge
Complications
- Meningitis
- Cavernous sinus thrombosis (ethmoid/sphenoid)
- Intracranial abscess
- Orbital cellulitis (ethmoid)
- Frontal bone osteomyelitis (Pott's puffy tumor)
- Extradural or subdural empyema
See Also
References
- ↑ Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, Cohen N, Cervin A, Douglas R, Gevaert P, Georgalas C, Goossens H, Harvey R, Hellings P, Hopkins C, Jones N, Joos G, Kalogjera L, Kern B, Kowalski M, Price D, Riechelmann H, Schlosser R, Senior B, Thomas M, Toskala E, Voegels R, Wang de Y, Wormald PJ. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinol Suppl. 2012 Mar;(23):3 p preceding table of contents, 1-298
- ↑ Chow AW et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Disease (2012) 54:e72-112.
- ↑ Trestioreanu AZ, Yaphe J. "Intranasal steroids for acute sinusitis." The Cochrane Database of Systematic Reviews. 2 December 2013. DOI: 10.1002/14651858.CD005149.pub4
- ↑ Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. IDSA Guidelines. 2012; Clinical Infectious Diseases e1-e41.






