Wide-complex tachycardia
(Redirected from Tachycardia (wide))
Background
- 3 wide complexes in a row is considered ventricular tachycardia
- Non-sustained if lasts < 30 seconds
- Sustained if lasts >30 seconds
Etiology[1][2][3]
- Due to true ventricular tachycardia in 80% of cases
- For patients with underlying cardiac disease, increases to > 90%
- Consider:
- Hyperkalemia
- Digoxin toxicity
- Severe metabolic acidosis
Clinical Features
- Depends on etiology
- Range from asymptomatic/palpitations to cardiac arrest
Differential Diagnosis
Narrow-complex tachycardia
- Regular
- AV Node Independent
- Sinus tachycardia
- Atrial tachycardia (uni-focal or multi-focal)
- Atrial fibrillation
- Atrial flutter
- Idiopathic fascicular left ventricular tachycardia
- AV Node Dependent
- AV Node Independent
- Irregular
- Multifocal atrial tachycardia (MAT)
- Sinus tachycardia with frequent PACs, PJCs, PVCs
- Atrial fibrillation
- Atrial flutter with variable conduction
- Digoxin Toxicity
Wide-complex tachycardia
Assume any wide-complex tachycardia is ventricular tachycardia until proven otherwise (it is safer to incorrectly assume a ventricular dysrhythmia than supraventricular tachycardia with abberancy)
- Regular
- Monomorphic ventricular tachycardia
- PSVT with aberrant conduction:
- PSVT with bundle branch block^
- PSVT with accessory pathway
- Atrial flutter with bundle branch block^
- Sinus tachycardia with bundle branch block^
- Accelerated idioventricular rhythm (consider if less than or ~120 bpm)
- Metabolic
- Irregular
- Atrial fibrillation/atrial flutter with variable AV conduction AND bundle branch block^
- Atrial fibrillation/atrial flutter with variable AV conduction AND accessory pathway (e.g. WPW)
- Atrial fibrillation + hyperkalemia
- Polymorphic ventricular tachycardia
^Fixed or rate-related
Evaluation
- Assume ventricular tachycardia until proven otherwise
Management
<translate>
Wide Regular Tachycardia[4]

Wide Regular Tachycardia (consistent with ventricular tachycardia).
Pulseless: see Adult pulseless arrest
- Unstable: Hypotension, altered mental status, shock, ischemic chest discomfort, acute heart failure
- Synchronized cardioversion 100-200J
- Stable:
- Medications
- Procainamide (first-line drug of choice)
- 20-50 mg/min until arrhythmia suppressed (max 17mg/kg or 1 gram); then, maintenance infusion of 1-4mg/min x 6hr
- Alternative administration: 100 mg q5min at max rate of 25-50 mg/min[5]
- Stop if QRS duration increases >50% or hypotension
- Avoid if prolonged QT or CHF
- Favored over Amiodarone in PROCAMIO trial; termination of tachycardia in 67% of procainamide group vs 38% of amiodarone group, adverse cardiac events 9% vs 41%, respectively [6]
- 20-50 mg/min until arrhythmia suppressed (max 17mg/kg or 1 gram); then, maintenance infusion of 1-4mg/min x 6hr
- Amiodarone (agent of choice in setting of AMI or LV dysfunction)
- 150 mg over 10min (15 mg/min), followed by 1 mg/min drip over 6hrs (360 mg total)[7]
- Then 0.5 mg/min drip over next 18 hrs (540 mg total)
- Oral dosage after IV infusion is 400 -800 mg PO daily
- Consider adenosine
- Consider for diagnosis and treatment, if rhythm is regular and monomorphic (see rhythm diagnosis in regular wide complex tachycardia)
- 6 mg IV as a rapid IV push followed by a 20 mL saline flush; repeat if required as 12 mg IV push
- Synchronized cardioversion (100J)
- Procainamide (first-line drug of choice)
</translate>
<translate>
Wide Irregular Tachycardia
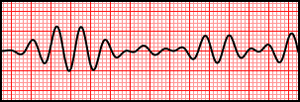
Wide Irregular Tachycardia (consistent with Torsades De Pointes).
- DO NOT use AV nodal blockers as they can precipitate V-Fib
- Pulseless: see Adult pulseless arrest
- Unstable: Hypotension, altered mental status, shock, ischemic chest discomfort, acute heart failure
- Unsynchronized cardioversion (defibrillation) 200J
- Stable:
- A fib with preexcitation
- 1st line - Electric Cardioversion
- 2nd line - Procainamide, amiodarone, or sotalol
- A fib with aberrancy
- Polymorphic V-Tach / Torsades De Pointes
- Give IV MgSO4
- Emergent defibrillation (NOT synchronized)
- Correct electrolyte abnormalities (esp hypoK, hypoMg)
- Stop prolonged QT meds
</translate>
Recurrent
- ≥3 episodes within 24 hours considered electrical storm and may require alternate treatment (i.e. beta blockade, sedation, ablation)
Other considerations
- True Vtach generally has rate >120bpm. If rate <120bpm or refractory to other therapy, consider other causes
- When in doubt, use cardioversion for treatment of regular WCT. In irregular WCT, consider Afib with WPW in which Procainamide is the treatment of choice
- In very wide complex (>0.2 msec) and <120 bpm in a patient with significant history, consider giving calcium chloride to treat hyperkalemia
- Consider Acidosis
- Sodium channel blockade (e.g. from benadryl, TCA, or cocaine toxicity) may cause very wide complex (>0.2msec) tachycardia with rate <120bpm
- Treat with sodium bicarbonate
- Lidocaine, Procainamide, Amiodarone all block Na channels and may result in asystole in patients with intrinsic or extrinsic Na-channel blockade
Disposition
- Admit all patients (even if converted to normal sinus rhythm in ED)
See Also
- ACLS: Tachycardia
- ACLS (Main)
- Rhythm diagnosis in regular wide complex tachycardia
- Paroxysmal supraventricular tachycardia
- Nonsustained ventricular tachycardia
- Polymorphic ventricular tachycardia
- Electrical storm
- In-Training Exam Review
External Links
References
- ↑ Gupta AK, Thakur RK. Wide QRS complex tachycardias. Med Clin North Am. 2001;85(2):245–66– ix–x.
- ↑ Akhtar M, Shenasa M, Jazayeri M, Caceres J, Tchou PJ. Wide QRS complex tachycardia. Reappraisal of a common clinical problem. Ann Intern Med. 1988;109(11):905–912.
- ↑ Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986;104(6):766–771.
- ↑ American Heart Association. Web-based Integrated Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care – Part 7: Adult Advanced Cardiovascular Life Support. ECCguidelines.heart.org
- ↑ Procainamide. GlobalRPH. http://www.globalrph.com/procainamide_dilution.htm.
- ↑ Ortiz M, Martín A, Arribas F, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J. 2017 May 1;38(17):1329-1335
- ↑ Amiodarone. GlobalRPH. http://www.globalrph.com/amiodarone_dilution.htm.



