ECG Basics: Difference between revisions
No edit summary |
No edit summary |
||
| Line 79: | Line 79: | ||
#(note: R :S ratio greater than 1 also in: 1.RBBB 2.WPW type A. 3. Post. Wall MI. 4.kids.) | #(note: R :S ratio greater than 1 also in: 1.RBBB 2.WPW type A. 3. Post. Wall MI. 4.kids.) | ||
== RBBB == | == [[RBBB]] == | ||
#QRS > 0.12 in limb leads | #QRS > 0.12 in limb leads | ||
| Line 87: | Line 87: | ||
[[File:RBBB.jpg|thumb|center|500px|RBBB]] | [[File:RBBB.jpg|thumb|center|500px|RBBB]] | ||
== LBBB == | == [[LBBB]] == | ||
#ST depression and TWI are common | #ST depression and TWI are common | ||
#QRS > 0.12 in limb leads | #QRS > 0.12 in limb leads | ||
| Line 117: | Line 117: | ||
Journal of Electrocardiology. Vol 43 (2010). 40-42. | Journal of Electrocardiology. Vol 43 (2010). 40-42. | ||
[[Category:Cards]] | |||
[[Category:Cards]] | |||
Revision as of 02:31, 13 January 2014
General
- 1 small box = 1mm = 0.04 sec = 40 miliseconds
- 5 small boxes = 1 big box = 5mm = 0.2 sec = 200 miliseconds
- Entire ECG strip is ~10 seconds
Intervals
| Interval | Time (s) | Boxes |
| PR | 0.12 - 0.20 | 3-5 |
| QRS | .06 - 0.10 | 1.5-2.5 |
| QTc | <0.44 | N/A |
Axis
- Cannot be measured if BBBs are present
- If up in leads 1 and AVF then normal axis
Q waves
- Significant if >1 box wide or if is 1/3 of entire QRS amplitude
- Early Repolarization:
- ST elevation most prominent in lat precord leads (V4-6) but no reciprocal changs
- T waves usually broad, tall (>5mm) & upright
- Limb leads may also have ST elevation, rarely >2 mm
T waves
- Normally upright in 1, 2, V3-V6
- Negative in AVR
- If is greater than 2/3 height of R wave then is abnormal
- Deep symmetrical inverted T waves:
- Left ventricle apical hypertrophy
- Raised ICP (e.g.SAH)
- Wellen's (MI)
- Paced rhythm
- BBB's or WPW
- Idiopathic
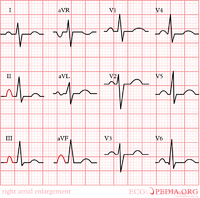
RAE
- Rarely isolated finding (usually RVH/RAD also)
- P amplitude >2.5mm in II
- Large biphasic p wave in V1
- Right atrial hyper.-initial component is larger in V1 than V6
- p-mitrale-m notched p wave in leads 1 and 2. Greater than .12 seconds.
LAE
- Biphasic P in V1 w/ wide, deep terminal component, >1mm depth & wide
- Left atrial hyper.-terminal component is larger than .04 sec.
LVH
- Sum of S in V1 or V2 & R in V5 or V6 is >35mm
- Sum of highest R & deepest S in precord is >45mm
- R wave in V6 > 18mm
- R in AVL of >12mm
- L precordial leads may show ST depression & TWI = LV strain pattern
- LAD-with slightly wide QRS. Or r in avl greater than 11mm, r in 1 is greater than 12mm, or R in AVf is greater than 20mm
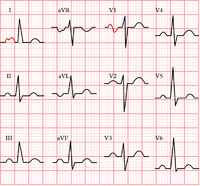
RVH
- Dominant R in V1 >7mm (also seen in WPW, RBBB, post MI, & nml var)
- RSR in V1 w/ QRS < 0.12
- This dx usu also w/ RAE or strain (ST dep w/ twi in V1-V3).
- Less sens. & spec. than LVH, usu nl ecg
- RVH-R wave greater than S in V1, but gets progressively smaller from V1 to V6. S wave persists in V5 and V6. RAD with slightly wide QRS.
- (note: R :S ratio greater than 1 also in: 1.RBBB 2.WPW type A. 3. Post. Wall MI. 4.kids.)
RBBB
- QRS > 0.12 in limb leads
- Triphasic QRS (rSR'), often w/ ST depression & TWI in V1-V3
- V1 must have a positive complex
- Slurred S in 1 and V6
LBBB
- ST depression and TWI are common
- QRS > 0.12 in limb leads
- Leads
- Large and wide R waves — leads I, aVL, V5, and V6
- Small R wave followed by deep S wave —leads II, III, aVF, V1–V3
LAFB
- Left axis deviation (-45 or more) w/QRS <0.10s
- Deep S in II, III, and AVF
LPFB
- Usually means disease
- Right axis deviation (>110) w/QRS < 0.10s
- Tall R in II, III, AVF
- Exclude other causes (COPD, RVH, Lat MI)
Low Voltage
- QRS < 5 mm in limb leads, or
- QRS < 10 mm in chest leads
- From either low electrical power within the heart (e.g. hypothyroidism), or low conduction within the heart (e.g. sarcoid or scar tissue), or poor conduction from the heart to the ECG lead (e.g. obesity, COPD, pericardial effusion
- Low voltage + tachycardia = pericardial effusion until proven otherwise
Source
8/19 Adapted from Niemann, Lampe, Pani, Donaldson, ECGpedia.org
Journal of Electrocardiology. Vol 43 (2010). 40-42.