Dengue: Difference between revisions
No edit summary |
|||
| Line 27: | Line 27: | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
{{ | {{Fever in Traveler DDX}} | ||
==Evaluation== | ==Evaluation== | ||
===Work-up=== | ===Work-up=== | ||
*Definitive testing | *Definitive testing | ||
**Reverse transcription polymerase chain reaction (RT-PCR) OR non-structural protein 1 (NS1) antigen tests, AND | **Reverse transcription polymerase chain reaction (RT-PCR) OR non-structural protein 1 (NS1) antigen tests, AND | ||
| Line 54: | Line 53: | ||
===Tourniquet Test=== | ===Tourniquet Test=== | ||
[[File:Tourniquettest.gif|thumbnail|Example of positive tourniquet test (right arm).]] | |||
*Tests for capillary fragility as a sign of ''Severe'' Dengue | *Tests for capillary fragility as a sign of ''Severe'' Dengue | ||
*Typically used in the absence of available [[DIC]] labs (i.e., low-resource settings) | *Typically used in the absence of available [[DIC]] labs (i.e., low-resource settings) | ||
Revision as of 21:05, 10 July 2024
Background

World map highlighting areas of dengue risk.[1]
- A viral infection transmitted though Aedes mosquitos typically in urban areas, especially during rainy seasons in tropical/subtropic regions (Asia, Africa, Central America, Caribbean)
- Also known as "break-bone fever"
- Most infections are asymptomatic or produce only mild illness, but the virus occasionally causes more severe cases up to death (i.e., "severe dengue")[2]
- Severe dengue (which includes "dengue shock syndrome") is rare in travelers, as it is cause by a second infection of a different Dengue serotype (so patients must have had two separate exposures at different times to be at risk)
Clinical Features
Dengue
- Incubation 3-7 days
- Febrile phase:
- High fever + 'Breakbone' + GI symptoms + rash + possible exposure
- +/- Faget sign
- Lasts 3-7 days, majority recover
Severe Dengue
As above, followed by:
- Critical Phase[3]:
- Minority of patients, generally pediatric and elderly
- Around time of defervescence
- Vascular leak, hypoproteinemia, hemoconcentration, pleural effusion, ascites
- Narrowed pulse pressure, persistent vomiting, RUQ tenderness, lethargy and restlessness are signs of impending collapse
- Mucosal and skin bleeding
Differential Diagnosis
Fever in traveler
- Normal causes of acute fever!
- Malaria
- Dengue
- Leptospirosis
- Typhoid fever
- Typhus
- Viral hemorrhagic fevers
- Chikungunya
- Yellow fever
- Rift valley fever
- Q fever
- Amebiasis
- Zika virus
Evaluation
Work-up
- Definitive testing
- Reverse transcription polymerase chain reaction (RT-PCR) OR non-structural protein 1 (NS1) antigen tests, AND
- IgM antibody tests
- For public health purposes, these tests may be ordered regardless of time since symptom onset
- May consider other tests to rule out other possible processes:
- CBC, chemistry, LFTs, viral panels
- If concern for Severe Dengue, add DIC labs
Diagnosis
- Typically a clinical diagnosis in the ED
- Definitive testing
- IgM diagnosed by a 4x increase in acute/ convalescent titers
- Other possible lab findings:
- CBC: Leukopenia, thrombocytopenia, and hemoconcentration
- CMP: LFTs elevated
- DIC lab abnormalities
- Severe Dengue if any of the following identified:
- Shock (from plasma leakage)
- Hemorrhage
- Respiratory distress
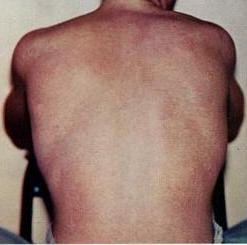
Tourniquet Test
- Tests for capillary fragility as a sign of Severe Dengue
- Typically used in the absence of available DIC labs (i.e., low-resource settings)
- Sensitivity of 52% and specificity of 82.4%
- A positive tourniquet test combined with lekuopenia increases sensitivity to 94%[4]
- Inflate cuff to pressure between SBP & DBP, and leave for 5 min
- (+) Test = 10-20 petechiae per square inch
Management
Dengue
- Supportive Care
- Acetaminophen for pain/fever
Severe Dengue
Above plus:
- IVFs
- Blood Transfusion - consider in hemorrhagic shock
Disposition
Dengue
- Typically outpatient, if well hydrated and non-toxic appearing
- May consider admitting certain high-risk patients (e.g., pregnant, extremes of age, concerning concomitant chronic disease)
Severe Dengue
- Typically admitted
- Consider ICU admission for patients with shock and end-organ damage
Prevention
- Vaccine available for the prevention of dengue virus and associated severe sequelae, Dengvaxia.[5]
- Only recommended for individuals 9-45 years old who have been infected once before with the virus[6].
- If patient has confirmed or likely dengue virus infection and they live and/or work in an endemic area, have them follow up with PCP for vaccination.
See Also
References
- ↑ CDC. July, 2024. https://www.cdc.gov/dengue/areas-with-risk/?CDC_AAref_Val=https://www.cdc.gov/dengue/areaswithrisk
- ↑ WHO website. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue#:~:text=There%20is%20no%20specific%20treatment%20for%20dengue.,often%20used%20to%20control%20pain.
- ↑ Simmons, C.P., Farrar, J.J., van Vinh Chau, N. and Wills, B. (2012) ‘Dengue’, New England Journal of Medicine, 366(15), pp. 1423–1432.
- ↑ Gregory CJ, Lorenzi OD, Colón L, García AS, Santiago LM, Rivera RC, Bermúdez LJ, Báez FO, Aponte DV, Tomashek KM, Gutierrez J, Alvarado L. Utility of the tourniquet test and the white blood cell count to differentiate dengue among acute febrile illnesses in the emergency room. PLoS Negl Trop Dis. 2011 Dec;5(12):e1400.
- ↑ Paz-Bailey G, Adams L, Wong JM, et al. Dengue Vaccine: Recommendations of the Advisory Committee on Immunization Practices, United States, 2021. MMWR Recomm Rep 2021;70(No. RR-6):1–16. DOI: http://dx.doi.org/10.15585/mmwr.rr7006a1
- ↑ Paz-Bailey G, Adams L, Wong JM, et al. Dengue Vaccine: Recommendations of the Advisory Committee on Immunization Practices, United States, 2021. MMWR Recomm Rep 2021;70(No. RR-6):1–16. DOI: http://dx.doi.org/10.15585/mmwr.rr7006a1