Pericardial effusion and tamponade
Revision as of 16:49, 21 June 2016 by Ostermayer (talk | contribs) (Text replacement - " pts" to " patients")
Background
- Always consider in pt w/ PEA
- Always consider in pt w/ myocardial stab wound (80% result in tamponade)
- GSW is less likely to result in tamponade b/c pericardial defect is larger
- Pathophysiology
- Increased pericardial pressure > decreased RV filling > decreased CO
Etiology
- Hemopericardium
- Trauma
- Iatrogenic (misplaced central line)
- Bleeding diathesis
- Ventricular rupture (post-MI)
- Non-hemopericardium
- Cancer - most commonly lung, breast
- Melanoma has predilection for heart
- May be related to radiation, infection, chemotherapy
- Pericarditis
- Infectious
- Uremic (renal failure)
- HIV complications (infection, Kaposi sarcoma, lymphoma)
- SLE
- Post-radiation
- Myxedema
- Cancer - most commonly lung, breast
Differential Diagnosis
Chest pain
Critical
- Acute coronary syndromes (ACS)
- Aortic dissection
- Cardiac tamponade
- Coronary artery dissection
- Esophageal perforation (Boerhhaave's syndrome)
- Pulmonary embolism
- Tension pneumothorax
Emergent
- Cholecystitis
- Cocaine-associated chest pain
- Mediastinitis
- Myocardial rupture
- Myocarditis
- Pancreatitis
- Pericarditis
- Pneumothorax
Nonemergent
- Aortic stenosis
- Arthritis
- Asthma exacerbation
- Biliary colic
- Costochondritis
- Esophageal spasm
- Gastroesophageal reflux disease
- Herpes zoster / Postherpetic Neuralgia
- Hypertrophic cardiomyopathy
- Hyperventilation
- Mitral valve prolapse
- Panic attack
- Peptic ulcer disease
- Pleuritis
- Pneumomediastinum
- Pneumonia
- Rib fracture
- Stable angina
- Thoracic outlet syndrome
- Valvular heart disease
- Muscle sprain
- Psychologic / Somatic Chest Pain
- Spinal Root Compression
- Tumor
Clinical Features
- CP, SOB, fatigue
- CHF-type appearance
- Narrow pulse pressure
- Friction rub
- Beck's Triad (33% of patients)
- Hypotension, muffled heart sounds, JVD
Diagnosis
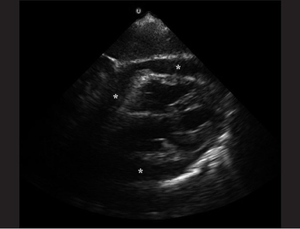
- Ultrasound
- Pericardial effusion
- In acute cases, even a relatively small build up of pericardial fluid can lead to hemodynamic compromise
- Diastolic collapse of the right atrium (in atrial diastole)
- Diastolic collapse of the right ventricle
- Plethoric IVC
- Valvular pulsus parodoxus
- Doppler interrogation across the mitral valve will demonstrate exaggerated respiratory variability of transvalvular flow
- Pericardial effusion
- ECG
- Can be normal
- Tachycardia (bradycardia is ominous finding)
- Electrical alternans
- Low voltage
- All limb lead QRS amplitudes <5 mm;[1]
- OR All precordial QRS amp <10 mm
- CXR
- Enlarged cardiac silhouette
- Pulsus Paradoxus
- >10mmHg change in systolic BP on inspiration
Treatment
Hemorrhagic Tamponade
- Pericardiocentesis
- Temporizing measure until thoracotomy can be performed
- IVF to increase RV volume
- Medications
Non-hemorrhagic Tamponade
- Pericardiocentesis
- Dialysis for patients with known renal failure
Disposition
- Admit with cardiology/CT surgery consult
See Also
Source
- ↑ Mattu A, Brady W. ECGs for the Emergency Physician 2, BMJ Books 2008.