Harbor: Base Hospital Resource for Physicians and MICNs
Harbor-UCLA Base Hospital
- This is intended as a quick reference for Harbor-UCLA Base Hospital Physicians and MICNs.
- For the most up to date guidelines, reference the LA County EMS Agency Prehospital Care Manual.
Los Angeles County Prehospital Care Manual and Treatment Protocols
Types of Incoming Base Hospital Radio Calls
- 1. Base Contact (Medical direction by MICN, Attending, R4, R3).
- Includes traumatic injury, cardiac arrest, termination of resuscitation in the field, AMA.
- 2. Base Notification (Medical direction by MICN, Attending, R4, R3).
- 3. Base to Base Referral (Medical direction by MICN or experienced Base Hospital Physician).
- 4. 911 Inter-facility Transport for Trauma (Attending Base Hospital Physician must take the report and accept patient).
- 5. 911 Inter-facility Transport for STEMI (Attending Base Hospital Physician must take the report and accept patient).
- 6. Multiple Casualty Incident (Medical direction by MICN or experienced Base Hospital Physician).
Common Provider Codes for Harbor-UCLA Base Hospital
- Most Commonly Used Provider Impression Codes
- ABOP = Abdominal Pain/Problems
- ETOH = Alcohol Intoxication
- ALOC = Altered Level of Conciousness-Not Hypoglycemia or Seizure
- PSYC = Behavioral/Psychiatric Crisis
- BRUE = BRUE
- CANT = Cardiac Arrest-Non-Traumatic
- CPNC = Chest Pain-Not Cardiac
- CPMI = Chest Pain-STEMI
- CPSC = Chest Pain-Suspected Cardiac
- DIZZ = Dizziness/Vertigo
- HYPR = Hyperglycemia
- HYTN = Hypertension
- HYPO = Hypoglycemia
- HOTN = Hypotension
- SOBB = Respiratory Distress/Bronchospasm
- RDOT = Respiratory Distress/Other
- CHFF = Respiratory Distress/Pulmonary Edema/CHF
- SEPI = Seizure-Postictal
- SEPS = Sepsis
- SHOK = Shock
- SYNC = Syncope/Near Syncope
- TRMA = Traumatic Injury
- WEAK = Weakness-General
- Common Paramedic Provider Agency Codes
- CF = Los Angeles County Fire
- CI = Los Angeles City Fire
- CM = Compton Fire
- MB = Manhattan Beach Fire
- RB = Redondo Beach Fire
- TF = Torrance Fire
- Most Common ECG Codes
- AFI = Atrial Fibrillation
- ASY = Asystole
- PEA = Pulseless Electrical Activity
- SR = Sinus Rhythm
- ST = Sinus Tachycardia
- VF = Ventricular Fibrillation
- VT = Ventricular Tachycardia
- Most Common Location Codes
- HO = Home
- NH = Nursing Home
- FR = Freeway
- ST = Street/Highway
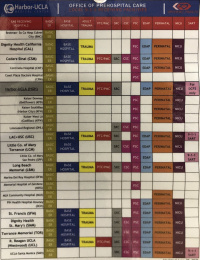
- Most Common 9-1-1 Receiving Hospital Codes
- CNT = Centinela Hospital
- HGH = Harbor UCLA Medical Center
- KFH = Kaiser South Bay
- LCM = Providence Little Company of Mary Medical Center - Torrance
- MHG = Gardena Memorial Hospital
- MLK = Martin Luther King Hospital
- TOR = Torrance Memorial
Specialized Care and Transport Considerations
STEMI
- Medical management according to TP 1211.
- Ensure Harbor-UCLA Medical Center is OPEN to STEMI by checking ReddiNet.
- ECG documentation (ECG section of the Base Contact Form).
- Initial Rhythm, 12-Lead ECG @ (time), EMS Interpretation, Software Interpretation.
- Obtain transmitted ECG from Harbor-UCLA STEMI outlook email.
- Discuss with Attending regarding STEMI page out and cath lab activation prior to patient arrival.
- Destination: STEMI Receiving Center (SRC)
Stroke
- Medical management according to TP 1232.
- On all patients exhibiting local neurologic signs, paramedics must perform and report:
- 1. Modified Los Angeles Prehospital Stroke Screen (mLAPSS)
- 2. If mLAPSS positive --> Document Los Angeles Motor Scale (LAMS) score (1 to 5) and Last Known Well Time (LKWT).
- MUST document mLAPSS +/- LAMS/LKWT on the Base Contact Form (Assessment Section) for provider impression Stroke/CVA/TIA (STRK).
- Prehospital stroke evaluation tools
- mLAPSS[1]: A decision tool designed to rapidly differentiate acute strokes that may benefit from expedited acute stroke therapy from stroke mimics in the field
- LAMS Score[2]: A validated score to predict large vessel occlusion in the field.
- LAMS ≥4 showed sn 81%, sp 89%, and overall accuracy 85% for predicting LVO.[3]
- Destination:
- If mLAPSS positive, LAMS 4-5, LKWT < 24 hours -> Transport to Comprehensive Stroke Center (CSC) if within 30 min.
- If mLAPSS positive, LAMS ≤ 3, LKWT < 24 hours -> Transport to closest Stroke Center (Primary or Comprehensive).
- mLAPSS negative but acute stroke suspected -> Transport destination is at the discretion of Base Hospital.
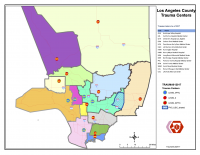
Traumatic Injury
- Medical management according to TP 1244 for adults, TP 1244-P for pediatrics.
- Any patient that meets trauma criteria or is deemed by provider judgment to meet trauma criteria should be transported to the nearest adult or pediatric trauma center.
- Trauma criteria can be found on the Base Contact Form under the TRAUMA and MECHANISM Sections. Patients are classified as a trauma patient if any of the red boxes are checked.
- Pediatric Trauma Center Criteria
- Children ≤14 years old should be transported to a Pediatric Trauma Center (PTC).
- Children >15 years old can be transported to an Adult Trauma Center (TC).
- Destination: Adult or Pediatric Trauma Center.
LA County Trauma Center Catchment Areas: Interactive GIS Map
Burns
- Medical management according to TP 1220 for adults and TP 1220-P for pediatrics.
- Major/critical burn criteria
- ≥ 15 years with 2nd and/or 3rd degree burn ≥ 20% TBSA.
- ≤ 14 years with 2nd and/or 3rd degree burn ≥ 10% TBSA.
- Destination:
- Major/critical burn that DOES NOT meet trauma center criteria -> Transport to Burn Center if it is more accessible than the Trauma Center.
- Major/critical burn that DOES meet trauma center criteria -> Transport to Trauma Center.
- Patient's burns DO NOT MEET major/critical burn criteria and DOES NOT meet trauma center criteria -> Transport to MAR.
- Los Angeles County Burn Centers
- LAC USC Medical Center
- Torrance Memorial Medical Center
- West Hills Hospital
Types of Destinations/Receiving Centers
- MAR = Most Accessible Receiving Facility
- TC = Adult Trauma Center
- EDAP = Emergency Department Approved for Pediatrics
- Think of an EDAP as a MAR for children approved for children ≤ 14 years old.
- PMC = Pediatric Medical Center
- Approved for critically ill children ≤ 14 years old.
- PTC = Pediatric Trauma Center
- Approved for children ≤ 14 years old who meet trauma criteria
- Perinatal Center
- Basic ED with 24/7 Obestrical services approved to care for pregnant patients >20 weeks gestation.
- SRC = STEMI Receiving Center
- PSC = Primary Stroke Center
- Able to care for most ischemic stroke cases
- CSC = Comprehensive Stroke Center
- Able to care for all ischemic and hemorrhagic stroke cases with 24/7 neurosurgery and minimally invasive catheter-based procedure capability including thrombectomy for large vessel occlusion.
Management of Non-Traumatic Cardiac Arrest and Termination of Resuscitation
- Medical management of non-traumatic cardiac arrest per TP 1210.
- Transport to SRC when transportation is indicated.
- Goal of OHCA resuscitation: Survival with good neurological outcome.
- Termination of Resuscitation:
- Non-shockable Rhythms (Aystole or PEA)
- If the patient remains in asystole after 20 minutes of EMS personnel CPR AND meets all of the following criteria, EMS personnel may determine death without base contact per Ref No. 814.
- 1. Patient 18 years or greater
- 2. Arrest not witnessed by EMS personnel
- 3. No shockable rhythm identified at any time during the resuscitation
- 4. No ROSC at any time during the resuscitation
- 5. No hypothermia
- If all these criteria are not met (including any PEA rhythm), base hospital physician consultation is required for the determination of death and termination of resuscitation in the field.
- If the patient remains in asystole after 20 minutes of EMS personnel CPR AND meets all of the following criteria, EMS personnel may determine death without base contact per Ref No. 814.
- Shockable Rhythms (Vfib or Vtach)
- Resuscitation should be continued for approximately 40 minutes on scene. Base hospital physician consultation is required for the determination of death and termination of resuscitation in the field.
- Non-shockable Rhythms (Aystole or PEA)
- Transportation without ROSC is discouraged.
- Special circumstances for transportation without ROSC include scene safety concerns, family disagreement with the decision to terminate resuscitation, and ongoing resuscitation inside the ambulance.
Base Contact For A Patient Refusing Transport
- See Ref No. 834
- In Los Angeles County, paramedics should not refuse transport and should honor any request by a patient for transport.
- AMA
- Adults
- Paramedics are required to make base contact for any patient leaving AMA.
- An adult with an ongoing medical emergency may refuse transport if they have decision-making capacity. The patient must be capable of understanding the risks of leaving AMA and be able to state these risks. It is highly recommended that the base hospital provider speak with the patient prior to leaving AMA.
- Consider asking the patient over the radio: "Do you understand that the risks and consequences of leaving against medical advice may be significant injury up to and including death?".
- For patients without decision-making capacity who are refusing transport, assistance from law enforcement should be requested by paramedics.
- Pediatrics
- Pediatric patients with an ongoing medical emergency should be transported under implied consent. If the parent or legal guardian refuses transport for a child with an ongoing medical emergency that requires transport, assistance from law enforcement should be requested.
- Adults
- Treat and Refer
- For patients without an ongoing medical emergency and with decision-making capacity, the patient may be released at the scene. Base contact is not required.
911 Trauma Re-Triage
- This system was developed to handle walk-in trauma patients to non-trauma centers or undertriage of trauma patients by EMS to non-trauma centers.
- The patient MUST meet one of the 8 defined criteria.
- Criteria #8: Patients, who in the judgment of the evaluating emergency physician, have a high likelihood of requiring emergent life- or limb-saving intervention within two hours.
- Consider that some interventions performed at the sending facility may be out of paramedic scope of practice (e.g. paralyzing agents, blood products, vasopressors, sedation medications). In these cases, the sending facility may be required to send a physician or nurse with the transport crew. Alternatively, interventions outside the paramedic scope of practice may be paused during transport if feasible.
- For patients who do not meet 911 Trauma Re-Triage criteria, consider MAC transfer.
Medications in Paramedic Scope of Practice in Los Angeles County
- It is important to remember that not all Los Angeles provider agencies stock all these medications and that each medication is only approved in the prehospital setting for specific indications.
- Approved ALS medications in Los Angeles County
- Adenosine
- Albuterol
- Amiodarone
- Aspirin
- Atropine
- Calcium Chloride
- Dextrose
- Diphenhydramine
- Epinephrine
- Fentanyl
- Glucagon
- Ketorolac
- Lidocaine
- Midazolam
- Morphine Sulfate
- Naloxone
- Nitroglycerin
- Ondansetron
- Oxygen
- Pralidoxime Chloride (DuoDote™)
- Sodium Bicarbonate
- See Ref No. 1300 for the approved prehospital indications for each medication.
ReddiNet
- A designated emergency and disaster communication system established for hospitals within Los Angeles County.
- Allows Los Angeles County hospitals to request diversion status, manage MCIs, and report bed availability.
- It is the responsibility of each hospital to ensure ReddiNet remains up to date and online at all times.
- Diversion requests categories
- Hospitals may request ED Saturation in 1 hour increments if unable to care for incoming ALS patients. BLS traffic is not diverted under ED Saturation.
- Other diversion categories include: CT Scanner, Trauma, Peds, STEMI, Stroke, Internal disaster (only category in which both ALS and BLS are diverted).
- See Ref No. 503.
Fundamental Concepts of On-line Medical Direction
- Criteria for paramedic base hospital contact per Ref No. 1200.2.
- In Los Angeles County, paramedics make base contact for specific provider impressions, after certain treatments or medications are administered, or in any case where further guidance is needed.
- Paramedics are licensed providers and able to practice independently based on established treatment protocols. This is also known as Off-line Medical Direction.
- On-line Medical Direction
- Occurs when paramedics contact the base hospital and base hospital physicians and MICNs direct paramedics to deliver treatments or interventions outside established protocols.
- Treatments or interventions MUST fall within paramedic scope of practice and should be evidenced-based.
- Direction can also be given to bypass a MAR if there is an indication to do so (e.g. Bypass MAR and transport to SRC if suspect possible STEMI but does not meet exact ECG STEMI criteria).
- When giving medication orders, be clear and direct, offer a brief explanation for your order/directive, and document clearly on the base hospital form (i.e. for PRN medication orders, remember to document dosage, route, and PRN indication).
- Additional education can always be provided on arrival.
Base Contact Form Documentation Reminders
- GEN INFO Section
- Document time in military time.
- Document weight in kgs.
- It is ok to approximate weight in kgs by dividing lbs by 2 (e.g. If medics state the patient is 100lbs, you can respond: "To confirm, the patient is 100 lbs or approximately 50 kgs").
- ASSESSMENT Section
- In select cases, it may be helpful to ask EMS personnel to obtain family contact information and/or bring along DNR/AHCD/POLST.
- PHYSICAL Section
- Document capnography # for all patients receiving positive pressure.
- VITALS & TXS Section
- Document a pain level when ordering PRN analgesia (ex. Morphine 4mg IV PRN pain >5/10).
- ECG Section
- If ECG was performed, ensure complete documentation of the initial Rhythm, 12-Lead ECG @ (time), EMS Interpretation, Software Interpretation.
- ARREST Section
- In cases of cardiac arrest, ensure complete documentation of the Rtn of Pulse (ROSC) @ (time) or Resus D/C @ (time) and Resus D/C Rhythm.
See Also
External Links
- LA County EMS Agency Prehospital Care Manual
- MDCalc - Los Angeles Motor Scale (LAMS)
- Time To Stop Beating A Dead Horse: Termination Of Resuscitation In The Field
References
- ↑ Kidwell CS, Starkman S, Eckstein M, et al. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000 Jan;31(1):71-6. doi: 10.1161/01.str.31.1.71. https://www.ahajournals.org/doi/pdf/10.1161/01.STR.31.1.71
- ↑ Llanes JN, Kidwell CS, Starkman S, Leary MC, Eckstein M, Saver JL. The Los Angeles Motor Scale (LAMS): a new measure to characterize stroke severity in the field. Prehosp Emerg Care. 2004 Jan-Mar;8(1):46-50. doi: 10.1080/312703002806. https://www.tandfonline.com/doi/abs/10.1080/312703002806
- ↑ Nazliel B, Starkman S, Liebeskind DS, et al. A brief prehospital stroke severity scale identifies ischemic stroke patients harboring persisting large arterial occlusions. Stroke. 2008;39(8):2264-2267. doi:10.1161/STROKEAHA.107.508127 https://www.ahajournals.org/doi/10.1161/STROKEAHA.107.508127