Laryngospasm: Difference between revisions
Elcatracho (talk | contribs) |
No edit summary |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
[[File:F5.png|thumb|Larynx as visualized from the hypopharynx.]] | |||
[[File:Cartilages and ligaments of the larynx.png|thumb|The cartilages and ligaments of the larynx seen posteriorly.]] | |||
[[File:F8.png|thumb|External views of the larynx: (a) anterior aspect; (b) anterolateral aspect with the thyroid gland and cricothyroid ligament removed.]] | |||
[[File:F6.png|thumb|Sagittal section through the head and neck showing the subdivisions of the pharynx.]] | |||
*An uncontrolled or involuntary muscular contraction of the vocal folds. | |||
*Reflex is normally triggered when the vocal cords or the area of the trachea below the vocal folds detects the entry of water, mucus, blood, or other substance. | |||
*Associated with [[ketamine]] (0.3%) | *Associated with [[ketamine]] (0.3%) | ||
**Usually associated with large doses or rapid IV push | **Usually associated with large doses or rapid IV push | ||
| Line 21: | Line 27: | ||
==Clinical Features== | ==Clinical Features== | ||
*Apnea may be the only sign in complete closure | *Apnea may be the only sign in complete closure | ||
*Partial closure can manifest as stridor, guttural noises, and paradoxical chest movement | *Partial closure can manifest as [[stridor]], guttural noises, and paradoxical chest movement | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
*Oversedation | |||
*Failure of respiratory drive | |||
==Evaluation== | ==Evaluation== | ||
| Line 40: | Line 47: | ||
*If above do not resolve laryngospasm, sedate more deeply ([[propofol]] is the traditional choice, 0.5mg/kg) | *If above do not resolve laryngospasm, sedate more deeply ([[propofol]] is the traditional choice, 0.5mg/kg) | ||
*If deeper sedation does not resolve laryngospasm, paralyze and intubate | *If deeper sedation does not resolve laryngospasm, paralyze and intubate | ||
*In pediatric patients, consider gentle chest compressions | |||
==Disposition== | ==Disposition== | ||
*Observation for 2-3 hours after resolution for development of post-obstructive pulmonary edema, bradycardia, or aspiration | *Observation for 2-3 hours after resolution for development of post-obstructive pulmonary edema, bradycardia (consider [[atropine]]), or aspiration | ||
==See Also== | ==See Also== | ||
Latest revision as of 15:31, 1 May 2024
Background
- An uncontrolled or involuntary muscular contraction of the vocal folds.
- Reflex is normally triggered when the vocal cords or the area of the trachea below the vocal folds detects the entry of water, mucus, blood, or other substance.
- Associated with ketamine (0.3%)
- Usually associated with large doses or rapid IV push
Causes
- Ammonia toxicity
- Medications
- Hypocalcemia
- Acute tetanus
- Ludwig's angina
- Acute laryngospasm
- Submersion injury
- Pulmonary chemical agents
- Pepper spray
- Smoke inhalation injury
- Caustic cocktail
Clinical Features
- Apnea may be the only sign in complete closure
- Partial closure can manifest as stridor, guttural noises, and paradoxical chest movement
Differential Diagnosis
- Oversedation
- Failure of respiratory drive
Evaluation
Workup
- Typically not indicated
Diagnosis
- Typically a clinical diagnosis
Management
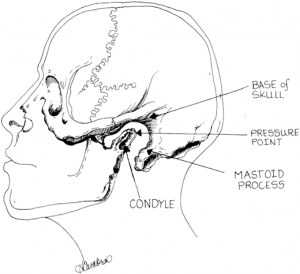
Apply pressure inwardly and anteriorly to the point labeled "Pressure Point" (Larson's Point) while applying a jaw thrust to relieve laryngospasm [1]
- Jaw thrust
- Place pressure on Larson's notch
- If jaw thrust and pressure are not sufficient, bag valve mask with PEEP
- If above do not resolve laryngospasm, sedate more deeply (propofol is the traditional choice, 0.5mg/kg)
- If deeper sedation does not resolve laryngospasm, paralyze and intubate
- In pediatric patients, consider gentle chest compressions
Disposition
- Observation for 2-3 hours after resolution for development of post-obstructive pulmonary edema, bradycardia (consider atropine), or aspiration
See Also
Airway Pages
- Pre-intubation
- Induction
- Intubation
- Surgical airways
- Post-intubation
External Links
References
- ↑ Larson CP Jr. Laryngospasm--the best treatment. Anesthesiology. 1998 Nov;89(5):1293-4. doi: 10.1097/00000542-199811000-00056. PMID: 9822036.






